Treatment of Kidney Failure
- Kidney failure can occur in one or both kidneys for a variety of reasons, such as
- Physical damage from an injury
- High blood pressure
- Diabetes
- Overuse of certain drugs (e.g. aspirin)
- Infection
- Kidney failure is dangerous and can be fatal within a relatively short time period
- Humans can survive with one functioning kidney
- If the kidneys fail urea is not excreted; this leads to a build-up of urea in the blood which can become toxic at high concentrations
- Kidney failure can also lead to disruption in the balance of water and solutes in the blood
- This can lead to problems relating to osmosis and cell damage as well as more specific problems relating to excess quantities of certain mineral ions
- There are two forms of treatment for kidney failure
- Dialysis
- Toxins, metabolic waste products and excess substances are removed from the blood by diffusion through a dialysis membrane
- Kidney transplant
- The non-functioning kidneys are replaced with a functioning kidney from a donor
- Note that the non-functioning kidneys are usually left in place while the new kidney is attached to the blood supply elsewhere in the abdomen
- Dialysis
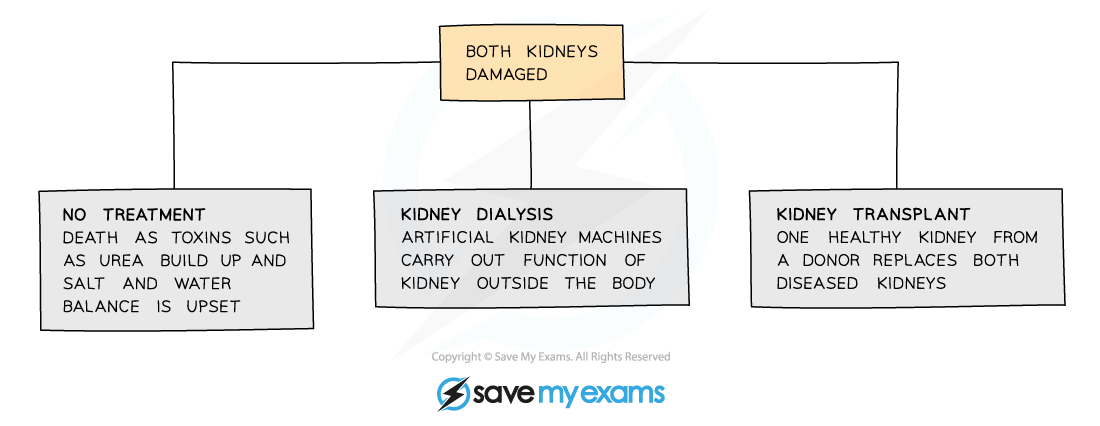
If both kidneys fail it can be fatal, but there are treatment options.
Haemodialysis
- Dialysis is a process used to separate small and large molecules with a partially permeable membrane
- Haemodialysis, also spelled hemodialysis, is a form of dialysis treatment that needs to be carried out several times a week and that requires a dialysis machine
- Another form of dialysis is known as peritoneal dialysis and involves use of the patient’s own internal membranes rather than a machine
- Blood flows via a tube from the patient to the dialysis machine
- Inside the dialysis machine partially permeable dialysis membranes separate the patient's blood from dialysis fluid
- Small molecules such as urea and salts can fit through pores in the dialysis membrane so exchange of substances can take place
- The dialysis fluid contains no urea, so there is always a urea diffusion gradient causing urea to diffuse out of the blood and into the fluid
- The dialysis fluid contains a salt concentration similar to the ideal blood concentration, so diffusion of salts across the membrane only occurs when there is an imbalance
- If the blood is too high in salts they will diffuse out of the blood and if the blood is too low in salts they will diffuse in
- The fluid contains a glucose concentration equal to normal blood sugar levels, preventing the outward diffusion of glucose across the membrane when blood glucose levels are normal
- If blood sugar levels are elevated the glucose will diffuse out of the blood into the fluid
- The blood and fluid flow in opposite directions to ensure a concentration gradient along the whole length of the membrane
- The fluid in the machine is also continually refreshed so that concentration gradients are maintained between the dialysis fluids and the blood
- This means that each time blood circulates through the machine some more of the urea it contains passes into the dialysis fluid, until almost all of it is removed
- Each haemodialysis session takes 3-4 hours to complete
- Patients are given a drug that prevents the formation of blood clots during dialysis
- Such drugs are known as anticoagulants
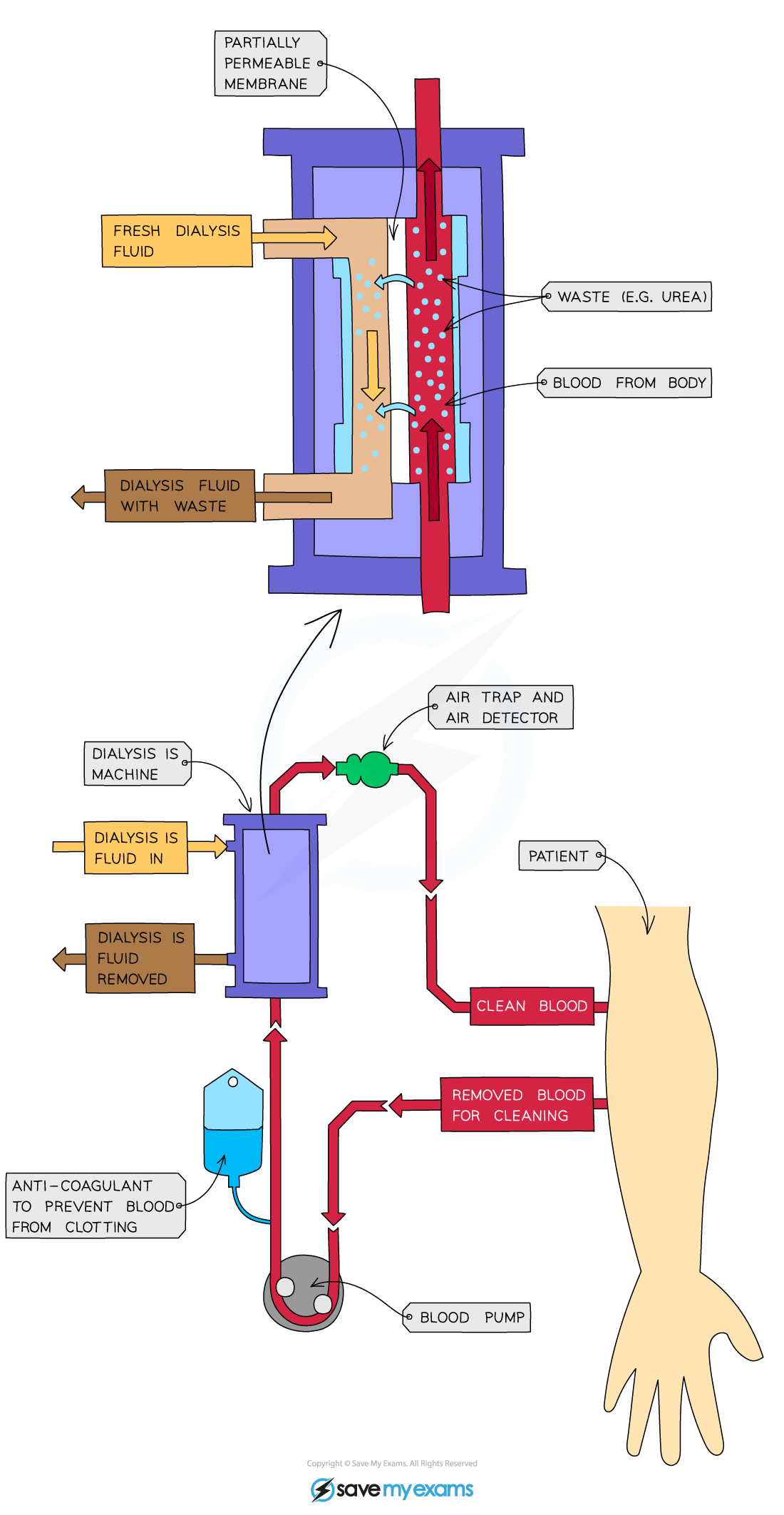
Haemodialysis involves passing blood through a dialysis machine, which enables removal of toxic urea and a rebalancing of water and solutes.
Kidney transplant
- An alternative to potentially restricting dialysis treatments is to have a kidney transplant
- This involves taking a single, healthy kidney from a donor and transplanting it into a patient with kidney failure
- Kidney transplants are considered to be a better long term solution to kidney failure than dialysis
- The patient has more freedom as they no longer need to have dialysis several times a week
- Patients often feel ill after dialysis and again as toxins start to accumulate a few days later; a transplant enables a patient to be healthy for an extended period
- Diet can be much less restricted than it needs to be when a patient is on dialysis
- There are still some risks associated with kidney transplants
- Donors won’t have the same antigens on their cell surface membranes as the patient so there will be some immune response to the new kidney
- Immunosuppressant drugs need to be taken for the rest of a patient’s life to reduce the risk of organ rejection; these can leave the patient vulnerable to infections
- A kidney will often be rejected over time, so a new kidney transplant is often needed after several years
- There are not enough donors to cope with the demand, and waiting lists are long
Urinalysis
- Analysing the composition of urine by carrying out urinalysis can tell us a great deal about the health of an individual; urine contains
- The products of metabolism
- Molecules that are present in the blood in high concentrations and that fit through the membranes in the glomerulus and Bowman's capsule
- Drugs that may have been taken into the body
- Urinalysis shows up any deviations from normal urine composition, aiding with medical diagnoses or detecting drug use
- Tests that can be carried out during urinalysis include
- pH testing
- The pH of urine may influence the development of kidney stones
- Test strips containing indicator chemicals may change colour when dipped in a urine sample
- Testing for glucose concentration
- High glucose levels in the urine can be a sign of diabetes
- Test strips similar to those used in pH testing can change colour to indicate the glucose concentration of a urine sample
- Testing for the presence of proteins
- In normal circumstances proteins are too large to filter through from the glomerulus, so if they are present in the urine this can be a sign of high blood pressure, kidney damage, or diabetes
- Drugs testing
- Drugs can be tested for using monoclonal antibodies which bind to specific drugs due to their complementary structure, showing up as a line on a test strip
- This kind of test works in a similar way to the lateral flow tests or rapid antigen tests that you may have come across when testing for COVID19
- This is important when testing for e.g. doping in sport
- Drugs can be tested for using monoclonal antibodies which bind to specific drugs due to their complementary structure, showing up as a line on a test strip
- Testing for the presence of white blood cells
- This can be a sign of infection in the urinary tract
- Pregnancy testing
- The hormones that circulate in the blood during pregnancy can be detected in the urine using complementary monoclonal antibodies
- pH testing
- An example of a type of urinalysis that involves a test strip and the use of monoclonal antibodies is the pregnancy test
- Pregnancy testing sticks contain antibodies that are specific to human chorionic gonadotropin (hCG), a hormone produced during pregnancy
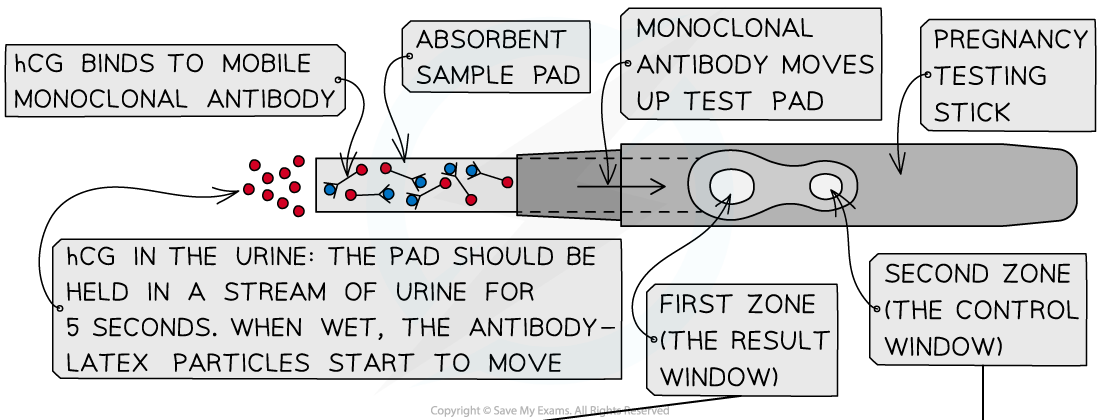
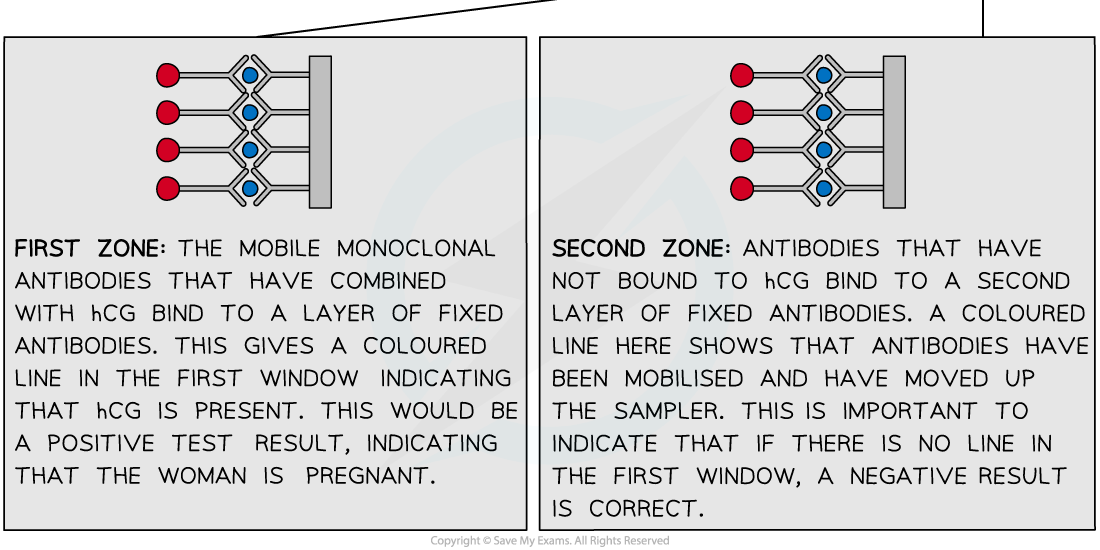
Monoclonal antibodies are used to detect the presence of the hormone hCG in the urine of pregnant women.
