Oestrogen & Progesterone
- During early development an embryo develops embryonic gonads that will either become ovaries in females or testes in males
- The factor that determines whether the embryonic gonads will develop into ovaries or testes is the presence or absence of a single gene known as the SRY gene
- The SRY gene is on the Y chromosome, so if the embryo has two X chromosomes the embryonic gonads will develop into ovaries
- This means testosterone will not be secreted by the developing embryo
- The two female hormones oestrogen and progesterone are present throughout pregnancy
- These hormones are secreted by the mother's ovaries and the placenta
- The absence of foetal testosterone and presence of maternal oestrogen and progesterone causes female reproductive organs to develop
- During female puberty, oestrogen and progesterone secretions increase.
- This leads to:
- The start of the menstrual cycle
- The development of female secondary sexual characteristics e.g. breast development
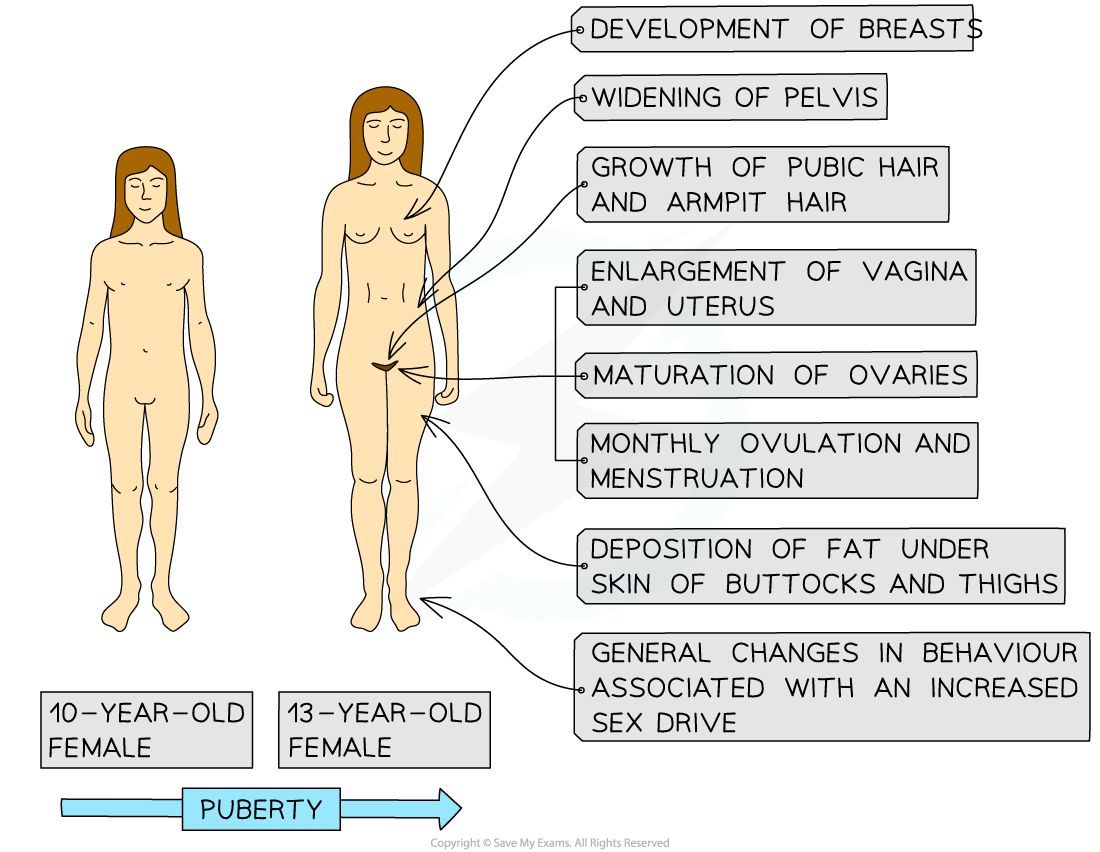
Secondary sexual characteristics of a human female
Menstrual Cycle
- The menstrual cycle is the series of changes that take place in the female body leading up to and following the release of an egg from the ovaries
- It starts in early adolescence in girls and is controlled by hormones
- The average menstrual cycle is 28 days long
- The uterus lining, or endometrium, thickens from day 7 through to day 28 of the cycle in preparation for receiving a fertilised egg
- The release of an egg, or ovulation, occurs about halfway through the cycle on day 14, and the egg then travels down the oviduct to the uterus
- Eggs develop inside fluid-filled sacs known as egg follicles inside the ovary
- The follicle releases the egg at ovulation and becomes an empty follicle known as a corpus luteum
- Failure to fertilise the egg leads to menstruation, commonly known as a period
- Menstruation involves the loss of menstrual blood via the vagina
- This is caused by the breakdown of the endometrium
- Menstruation takes place roughly between days 1-7 of the cycle
- The number of days during which menstruation occurs can vary
- After menstruation finishes, the endometrium starts to thicken again in preparation for the possible implantation of a fertilised egg in the next cycle
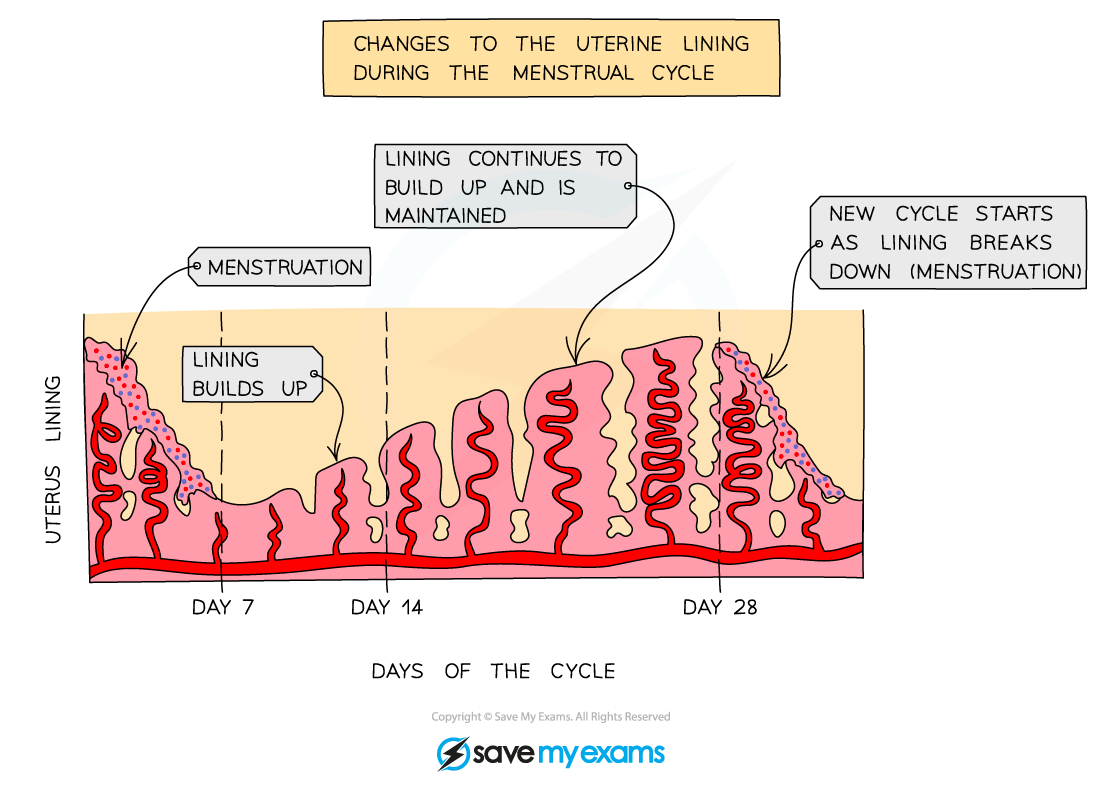
Changes in the endometrium during the menstrual cycle
How ovarian and pituitary hormones control the menstrual cycle
- Four hormones control the events that occur during the menstrual cycle:
- Two of these hormones are produced by the pituitary gland in the brain
- Follicle-stimulating hormone (FSH)
- Luteinising hormone (LH)
- The other two hormones are produced in the ovaries
- Oestrogen; produced by the egg follicle, and by the corpus luteum after ovulation
- Progesterone; produced by the corpus luteum
- Two of these hormones are produced by the pituitary gland in the brain
- The roles of FSH and LH:
- FSH is secreted by the pituitary gland and stimulates the development of several immature egg cells in follicles in the ovary
- FSH also stimulates the secretion of oestrogen by the follicle wall
- The pituitary gland is stimulated to release LH when oestrogen levels have reached their peak
- LH causes ovulation to occur; the shedding of the mature egg cell from the follicle and its release from the ovary
- The shedding of the mature egg cell leaves behind an empty egg follicle called the corpus luteum
- LH also stimulates the production of progesterone from the corpus luteum
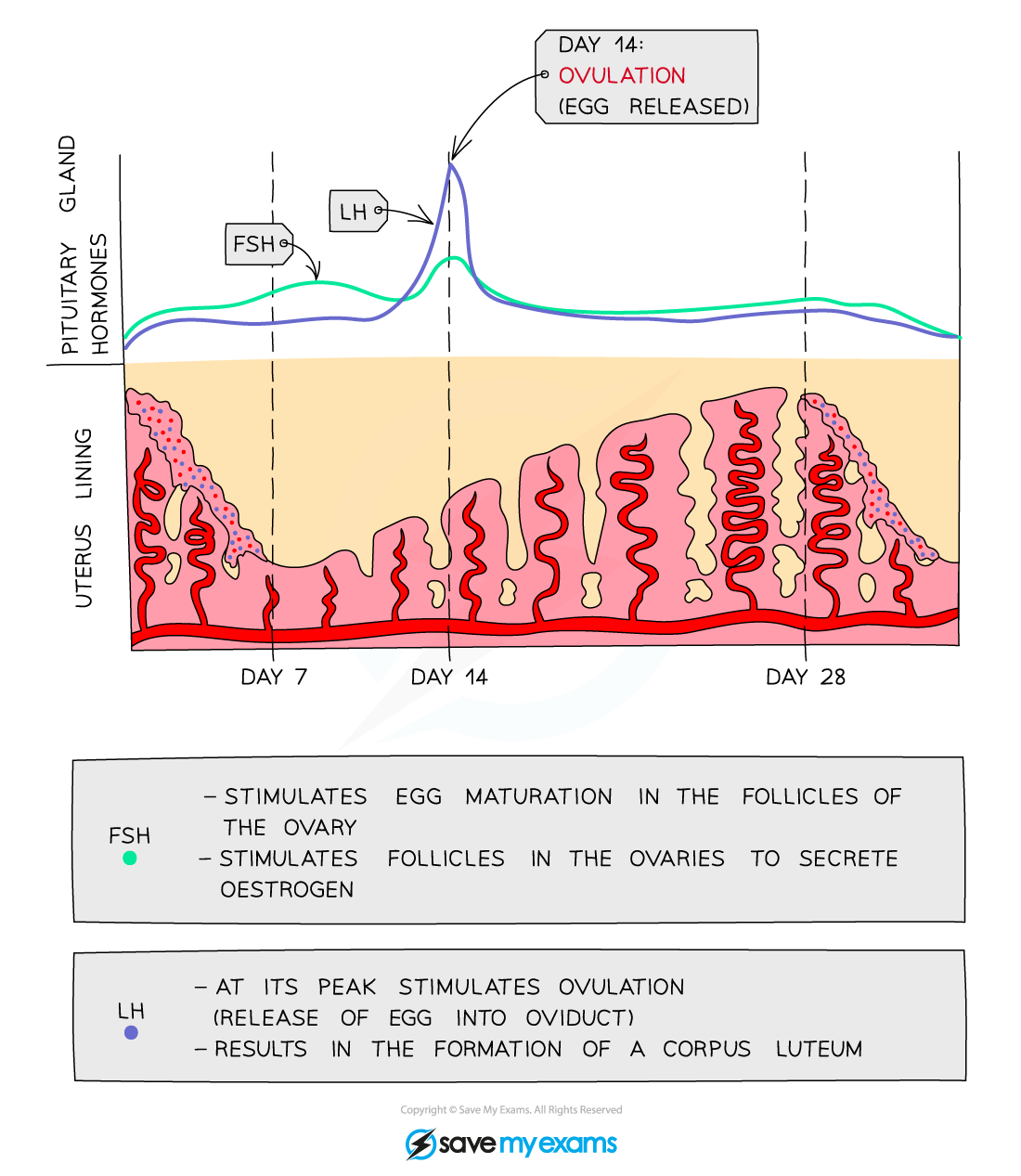
Changes in the levels of the pituitary hormones FSH and LH in the blood during the menstrual cycle
- The roles of oestrogen and progesterone:
- Oestrogen levels rise from day 1 to peak just before day 14
- This causes the endometrium to start thickening and the egg cell to mature
- The peak in oestrogen occurs just before the egg is released
- Progesterone stays low from day 1-14 and starts to rise once ovulation has occurred
- Progesterone is produced by the corpus luteum
- The increasing levels of progesterone cause the endometrium to continue to thicken
- A fall in progesterone levels as the corpus luteum deteriorates causes the endometrium to break down, resulting in menstruation
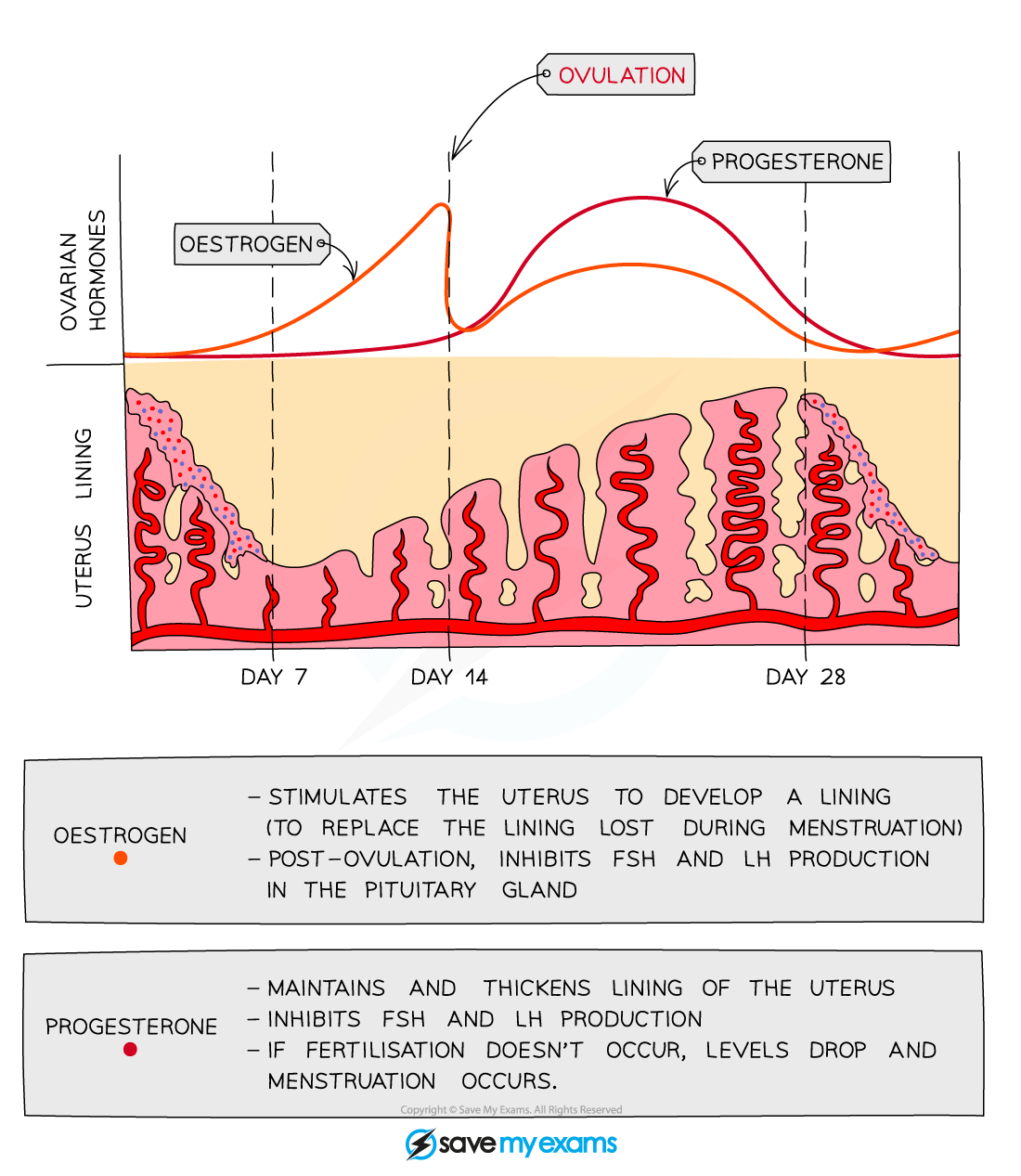
Changes in the levels of oestrogen and progesterone in the blood during the menstrual cycle
Negative and positive feedback mechanisms controlling the menstrual cycle
- The four hormones all interact to control the menstrual cycle via both negative and positive feedback
- FSH and oestrogen
- FSH stimulates the development of a follicle, and the follicle wall produces the hormone oestrogen; it can be said that FSH stimulates the production of oestrogen
- As well as causing growth and repair of the endometrium, oestrogen also causes an increase in FSH receptors; this makes the follicles more receptive to FSH which, in turn, stimulates more oestrogen production
- This is positive feedback
- When oestrogen levels are high enough, it inhibits the secretion of FSH
- This is negative feedback
- LH and oestrogen
- When oestrogen rises to a high enough level, it stimulates the release of LH from the pituitary gland, causing ovulation on around day 14 of the cycle
- After ovulation, LH causes the wall of the follicle to develop into the corpus luteum, which secretes more oestrogen
- This is positive feedback
- LH and progesterone
- LH stimulates the wall of the follicle to develop into the corpus luteum, which secretes progesterone
- Progesterone thickens and maintains the endometrium but also inhibits the secretion of FSH and LH from the pituitary gland
- This is negative feedback
- FSH and oestrogen
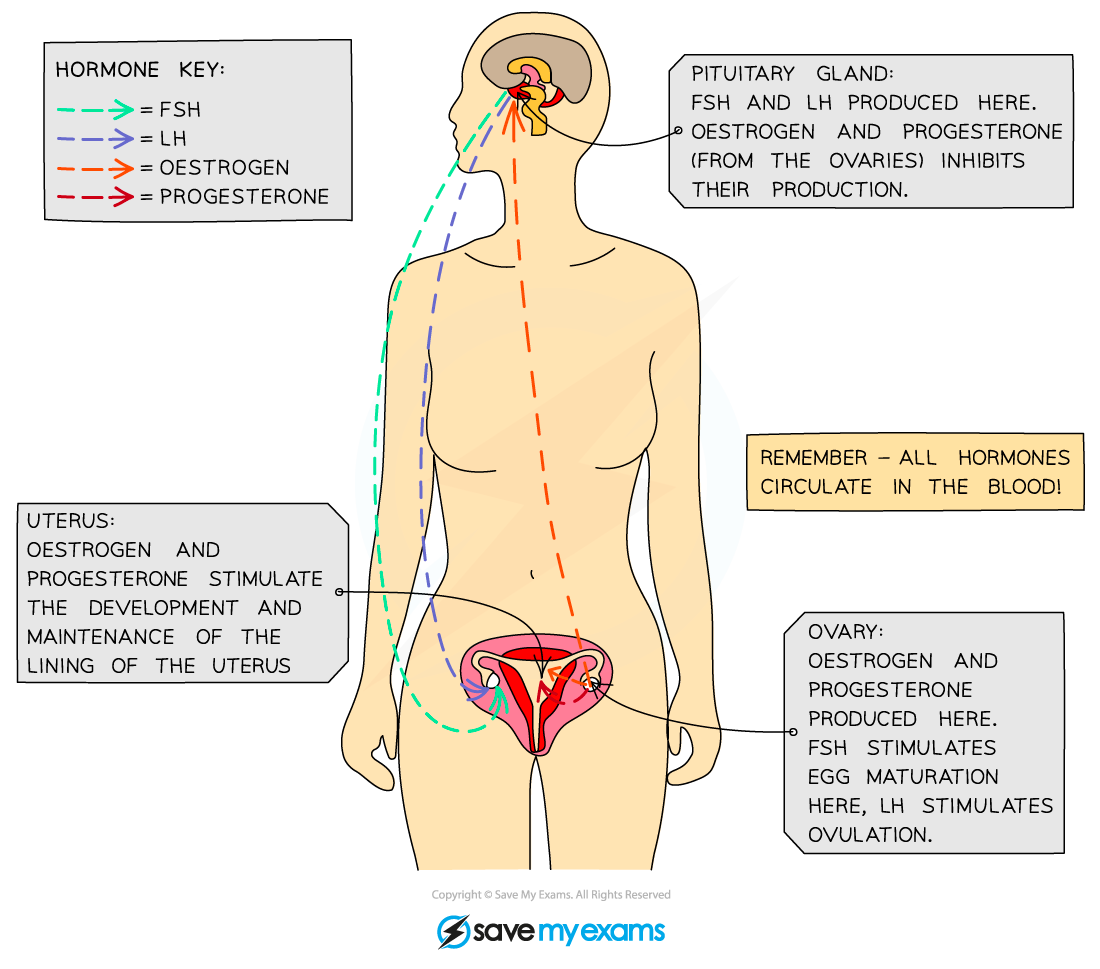
Where hormones involved in the menstrual cycle are made and act - remember that hormones travel around the body in the bloodstream but only have an effect on a target organ
Hormones & IVF
- A couple may find it difficult to conceive a baby naturally
- This can be due to insufficient levels of reproductive hormones affecting the development of egg and sperm cells, or as a result of issues with the reproductive system of the male or female
- One possible treatment is for eggs to be fertilised by sperm outside the body in carefully controlled laboratory conditions
- This is known as in vitro fertilisation, or IVF
- Although the process can vary, it normally follows the same main steps:
- The first step involves stopping the normal secretion of hormones; the woman takes a drug to inhibit the secretion of FSH and LH from the pituitary gland
- This also causes oestrogen and progesterone secretions to stop
- The first step involves stopping the normal secretion of hormones; the woman takes a drug to inhibit the secretion of FSH and LH from the pituitary gland
- This temporarily halts the menstrual cycle, allowing doctors to control the timing and quantity of egg production in the woman's ovaries
- The woman is then given injections of FSH and LH to stimulate the development of follicles; as the injection gives a much higher FSH concentration than is present during a normal menstrual cycle, 'superovulation' occurs
- Many more follicles than normal begin to mature
- The eggs are then collected from the woman and fertilised by sperm from the man in sterile conditions in the laboratory
- The fertilised eggs develop into embryos
- At the stage when they are tiny balls of cells, about 48 hours after fertilisation, one or more embryos are inserted into the mother’s uterus
- Finally, extra progesterone is normally given to the woman to ensure the endometrium is maintained
