Ultrastructure of the Glomerulus and Bowman's Capsule
Introduction to kidney structure
- Humans have two kidneys, which remove waste products from the blood and maintain the blood's balance of water and solutes
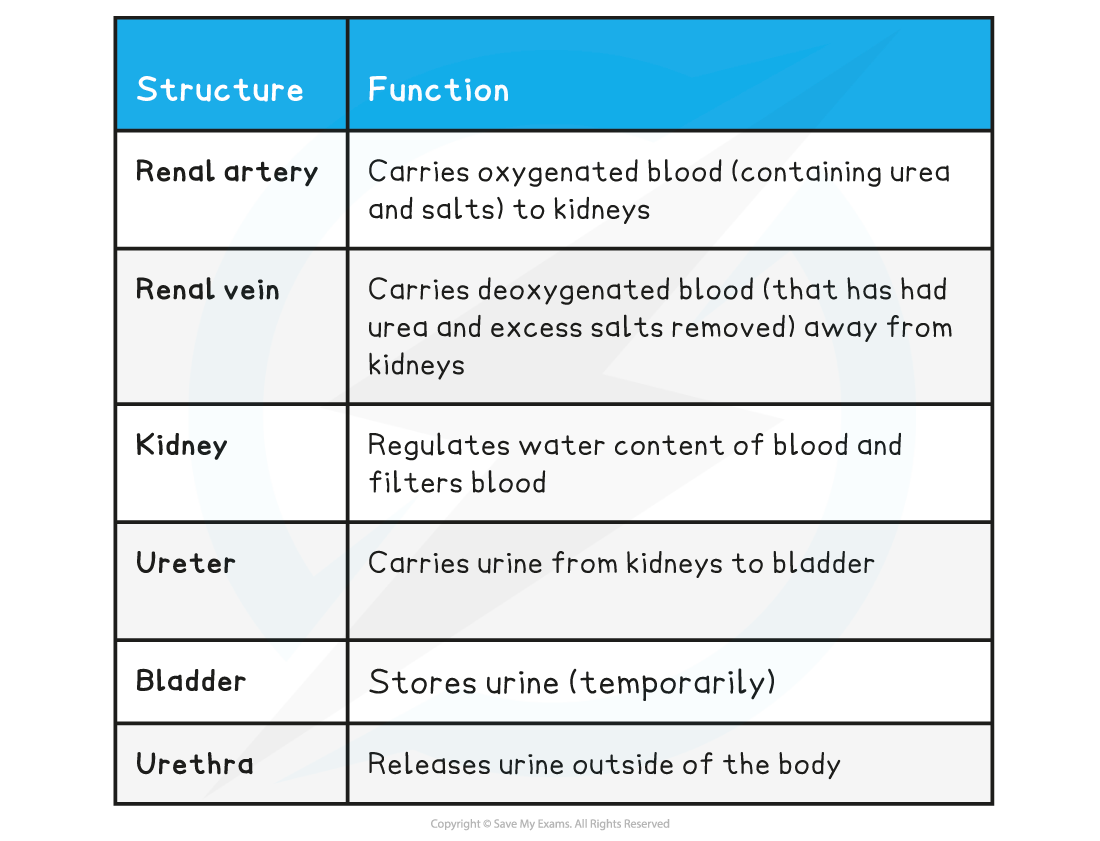
- The renal artery supplies blood to the kidneys, while the renal vein carries blood away
- The filtrate produced by the kidneys forms urine which is transferred to the bladder via a tube called the ureter
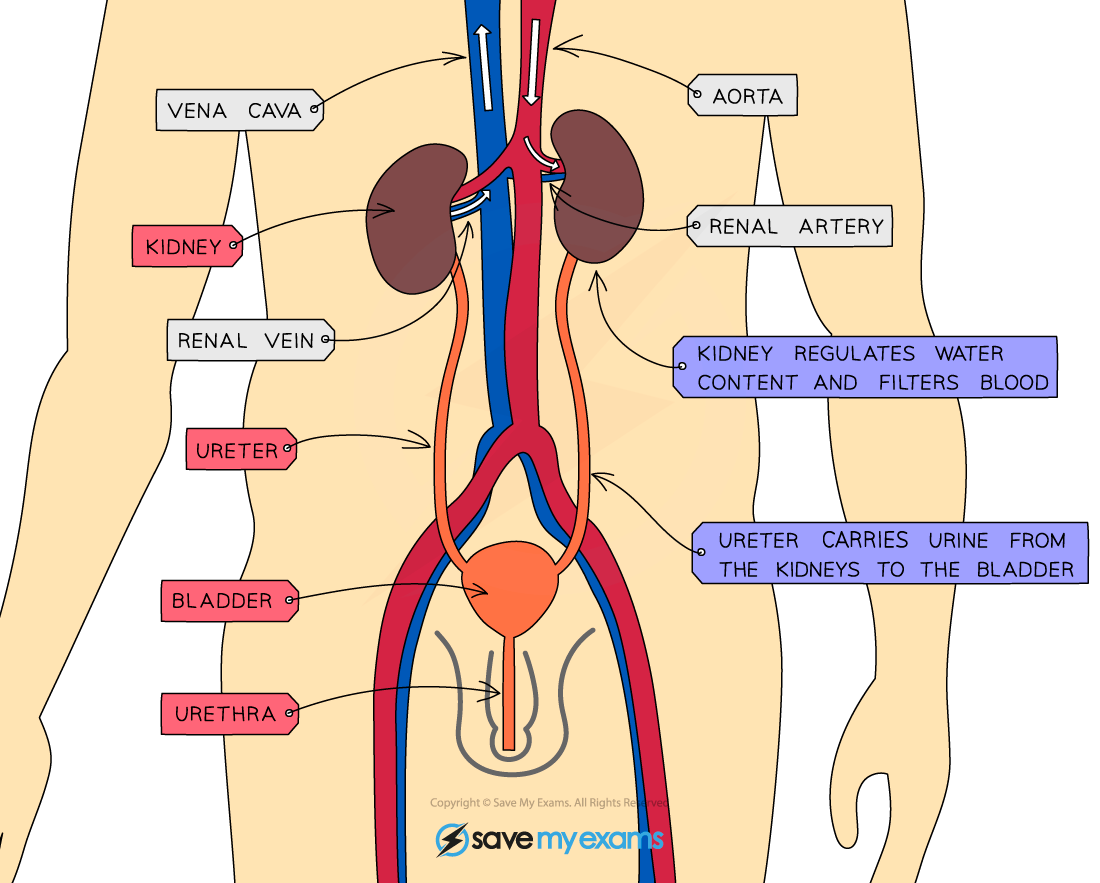
The kidneys are supplied with blood by the renal artery, while the renal vein carries blood away. A ureter carries urine from each kidney to the bladder.
Kidney Structure & Function Table
- The kidney itself is surrounded by an outer layer known as the fibrous capsule
- Beneath the fibrous capsule, the kidney has three main regions
- The cortex
- The medulla
- The renal pelvis

The kidney has three main regions; the cortex, the medulla, and the renal pelvis.
- Each kidney contains thousands of tiny tubes, or tubules, known as nephrons
- Nephrons are the functional unit of the kidney and are responsible for the formation of urine
- Different parts of the nephron are found in different regions of the kidney
- The cortex
- Location of the glomerulus, Bowman’s capsule, proximal convoluted tubule, and distal convoluted tubule
- The medulla
- Location of the loop of Henle and collecting duct
- The renal pelvis
- All kidney nephrons drain into this structure, which connects to the ureter
- The cortex


The nephron spans the three regions of the kidney.
The Glomerulus and Bowmans Capsule
- Within the Bowman’s capsule of each nephron is a structure known as the glomerulus
- Each glomerulus is supplied with blood by an afferent arteriole which carries blood from the renal artery
- The afferent arteriole splits into a ball of capillaries that forms the glomerulus itself
- The capillaries of the glomerulus rejoin to form the efferent arteriole
- Blood flows from the glomerulus into a network of capillaries that run closely alongside the rest of the nephron and eventually into the renal vein

The afferent arteriole supplies the capillaries of the glomerulus, which rejoin to form the efferent arteriole.
- The glomerulus sits within the Bowman's capsule; these two structures together carry out the process of ultrafiltration
- The blood in the glomerulus is at high pressure
- The afferent arteriole is wider than the efferent arteriole, increasing the blood pressure as the blood flows through the glomerulus
- Note that while all capillaries exert outward pressure, forcing tissue fluid out towards the surrounding cells, the outward pressure in the glomerulus is much higher than in other capillaries
- This high pressure forces small molecules in the blood out of the capillaries of the glomerulus and into the Bowman’s capsule
- These small molecules include
- Chloride ions
- Sodium ions
- Glucose
- Urea
- Amino acids
- These small molecules include
- The resulting fluid in the Bowman's capsule is called the glomerular filtrate
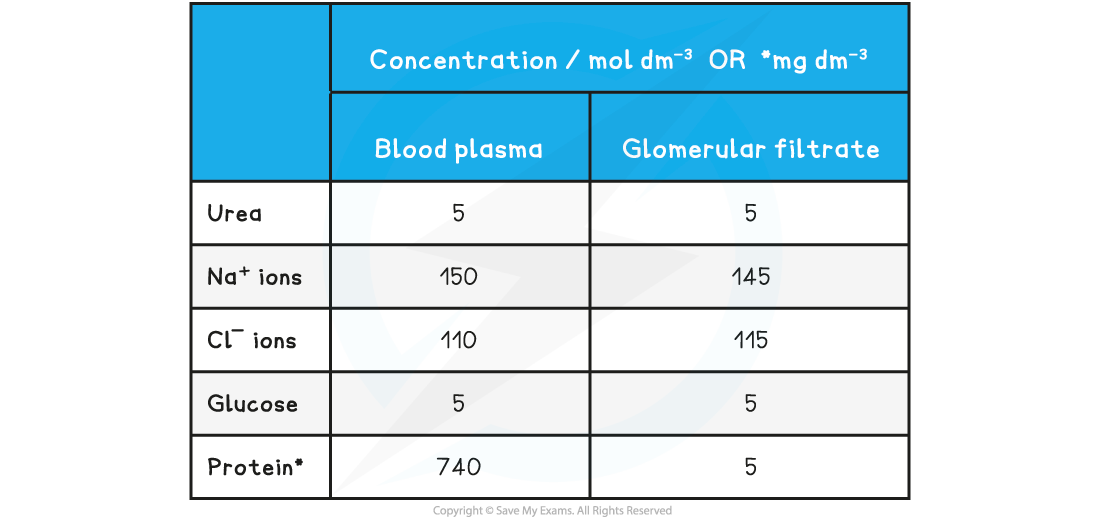
- Large molecules such as proteins remain in the blood and do not pass into the filtrate
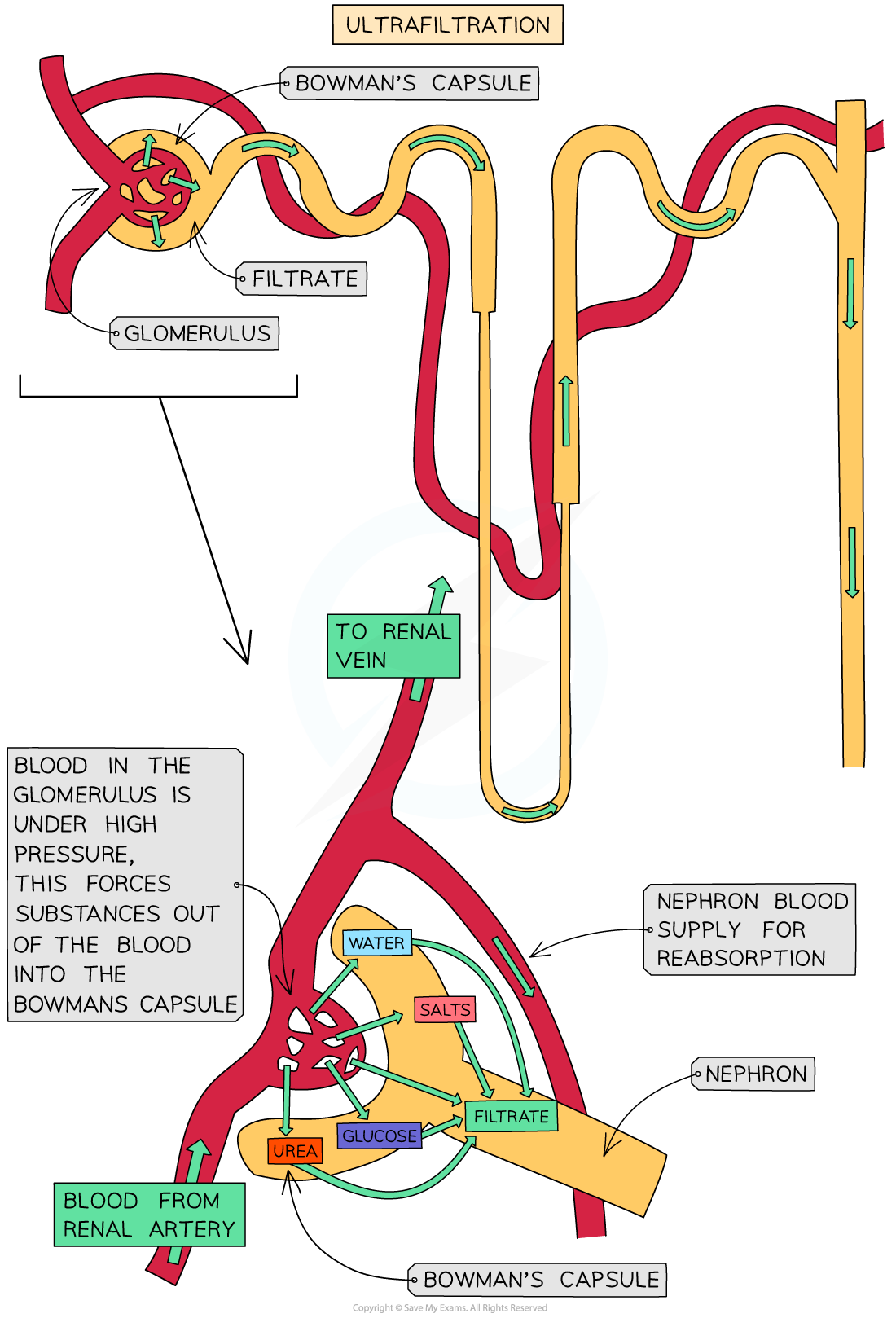
High blood pressure in the glomerulus forces small molecules into the Bowman's capsule, forming glomerular filtrate; this is ultrafiltration
Composition of the blood plasma compared to glomerular filtrate table
- The structures within the glomerulus and Bowman's capsule are especially well adapted for ultrafiltration
- The blood in the glomerular capillaries is separated from the lumen of the Bowman’s capsule by two cell layers with a basement membrane in between them:
- The first cell layer is the endothelium of the capillary
- There are gaps between the cells of the capillary endothelium known as fenestrations; fluid can pass through these gaps but not blood cells
- The next layer is the basement membrane
- The basement membrane is made up of a network of collagen protein and glycoproteins
- This mesh-like structure acts as a sieve, allowing small molecules through but preventing passage of large proteins from the blood plasma
- The second cell layer is the epithelium of the Bowman’s capsule
- The epithelial cells have many foot-like projections which wrap around the capillary; these cells are known as podocytes and the gaps between the projections allow the passage of small molecules
- The first cell layer is the endothelium of the capillary
- As blood passes through the glomerular capillaries the fenestrations between the capillary endothelial cells, the mesh-like basement membrane, and the gaps between the podocyte projections allow substances dissolved in the blood plasma to pass into the Bowman’s capsule
- The substances that pass into the Bowman’s capsule make up the glomerular filtrate
- The main substances that form the glomerular filtrate are amino acids, water, glucose, urea and salts (Na+ and Cl- ions)
- Red and white blood cells and platelets remain in the blood as they are too large to pass through the fenestrations between the capillary endothelial cells
- The basement membrane stops large protein molecules from getting through
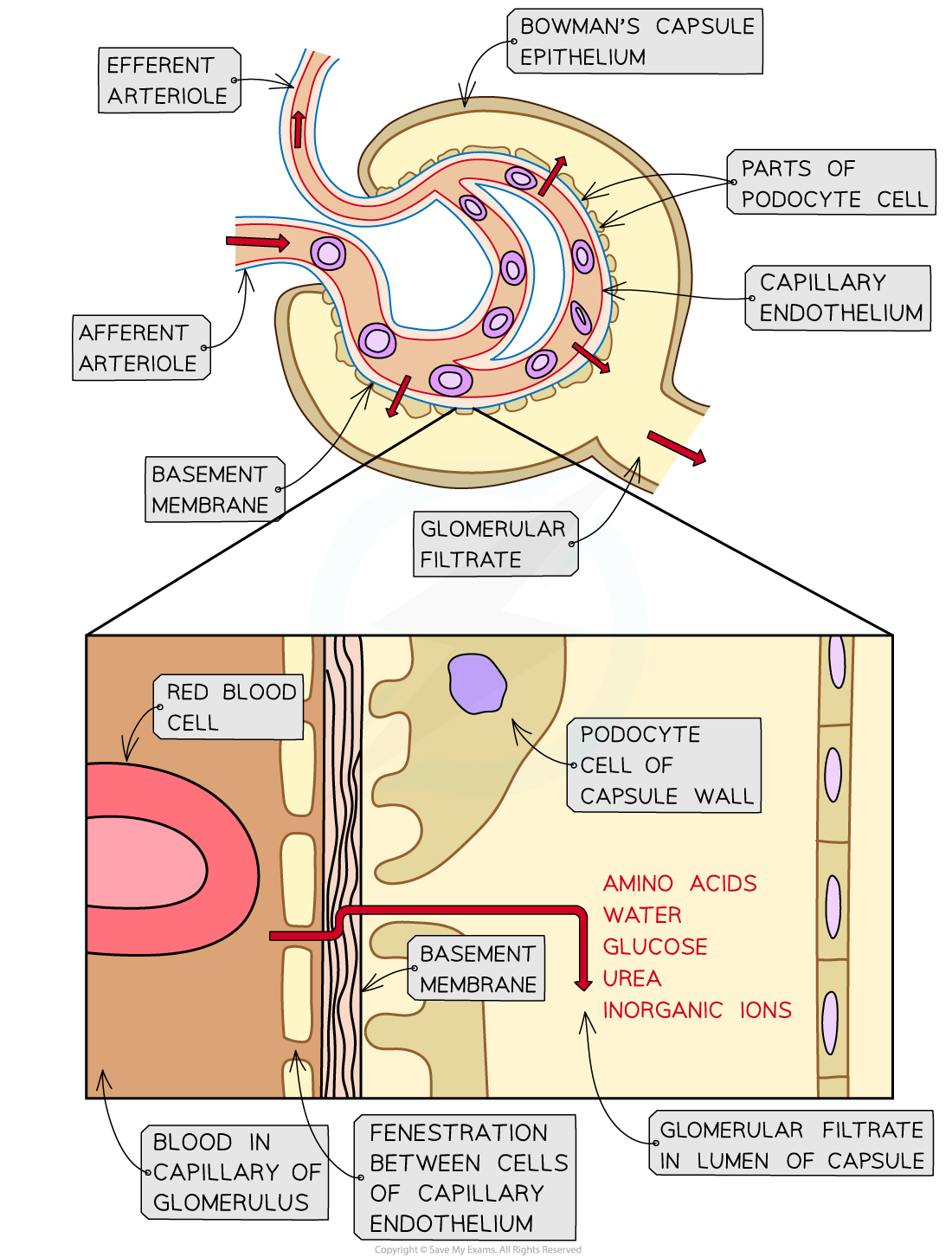
The glomerular filtrate must pass through three layers during ultrafiltration; the capillary endothelium, the basement membrane, and the Bowman’s capsule epithelium
Role of the Proximal Convoluted Tubule
- Many of the substances that pass into the glomerular filtrate are useful to the body
- These substances are therefore reabsorbed into the blood as the filtrate passes along the nephron
- This process is known as selective reabsorption since not all substances are reabsorbed
- Reabsorbed substances include water, salts, glucose, and amino acids
- Most of this reabsorption occurs in the proximal convoluted tubule
- Note that while most water and salts are reabsorbed in the proximal convoluted tubule, the loop of Henle and collecting duct are also involved in the reabsorption of these substances
- The lining of the proximal convoluted tubule is composed of a single layer of epithelial cells which are adapted to carry out reabsorption in several ways:
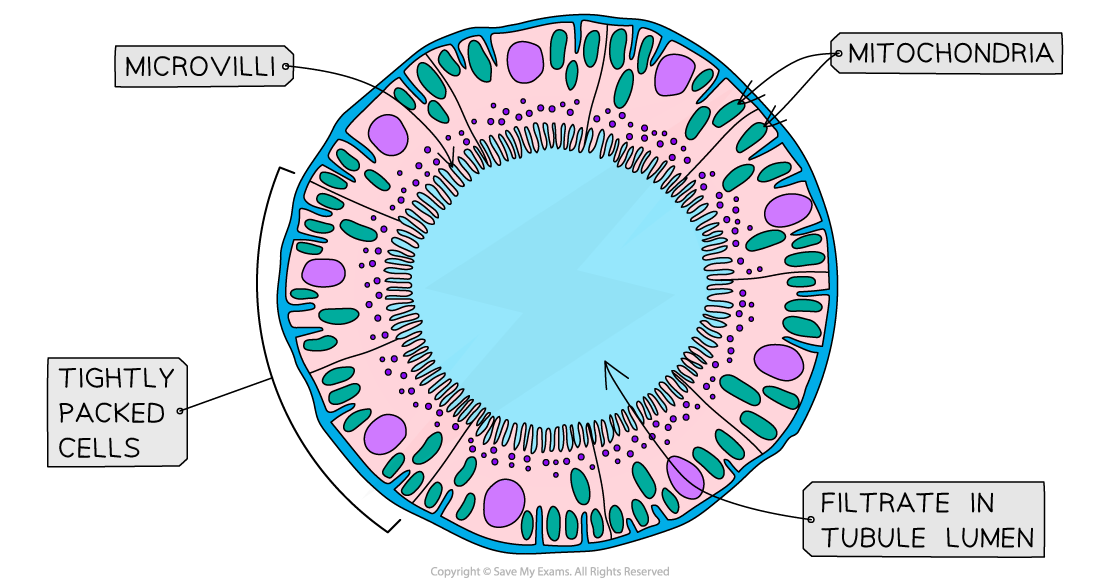
The proximal convoluted tubule, seen here in cross section, has several adaptive features to aid selective reabsorption
-
- Microvilli
- Microvilli are tiny finger-like projections on the surface of epithelial cells which increase the surface area for diffusion
- Co-transporter proteins
- Many mitochondria
- Tightly packed cells
- Microvilli
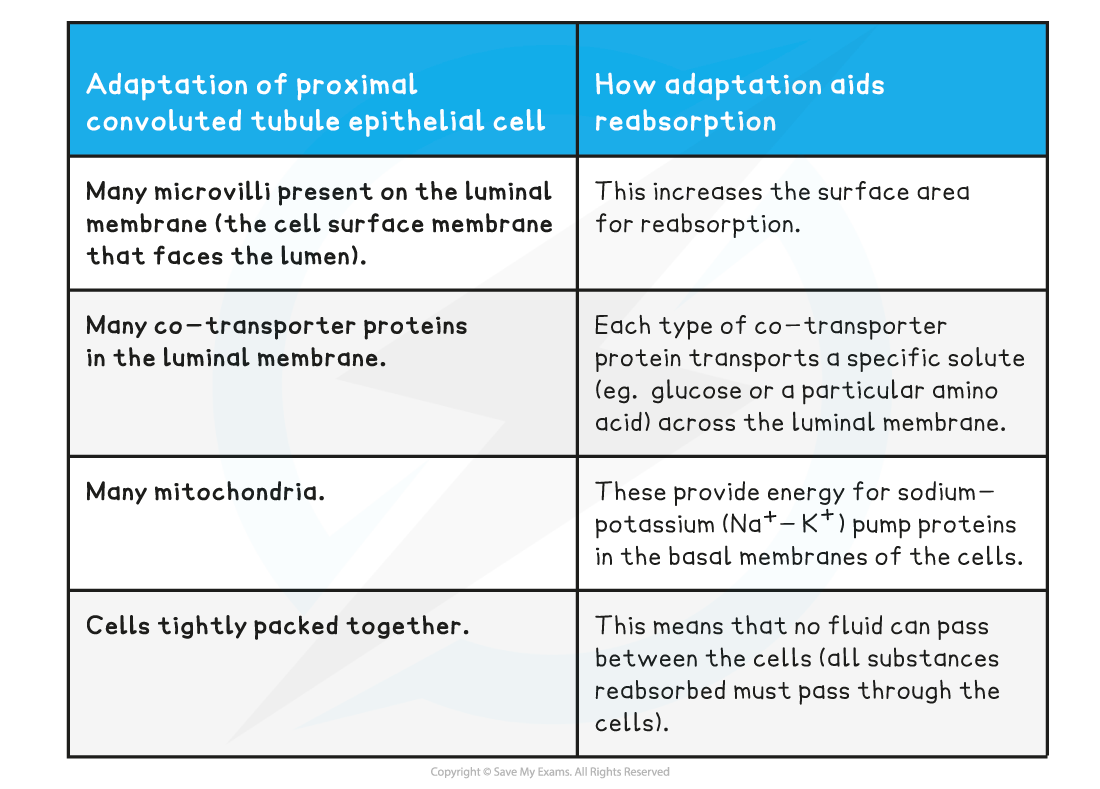
The process of selective reabsorption
- Sodium ions (Na+) are transported from the proximal convoluted tubule into the surrounding tissues by active transport
- The positively charged sodium ions creates an electrical gradient, causing chloride ions (Cl-) to follow by diffusion
- Sugars and amino acids are transported into the surrounding tissues by co-transporter proteins, which also transport sodium ions
- The movement of ions, sugars, and amino acids into the surrounding tissues raises the osmolarity of the tissues, so water leaves the proximal convoluted tubule by osmosis
- Urea moves out of the proximal convoluted tubule by diffusion
- All of the substances that leave the proximal convoluted tubule for the surrounding tissues eventually make their way into nearby capillaries down their concentration gradients
Role of the Loop of Henlé
- Many animals deal with the excretion of the toxic waste product urea by dissolving it in water and excreting it
- While this method of excretion works well, it brings with it the problem of water loss
- The role of the loop of Henle is to enable the production of urine that is more concentrated than the blood, and to therefore conserve water
- Note that it is also possible to produce urine that is less concentrated than the blood; this is important when water intake is high to prevent blood becoming too dilute
- The loop of Henle achieves this by the use of a countercurrent multiplier system
- Countercurrent refers to the opposite directions of filtrate flow in the descending and ascending limbs of the loop of Henle
- Multiplier refers to the steep concentration gradient that the loop of Henle is able to generate across the medulla
The process in the loop of Henle
- Sodium and chloride ions are pumped out of the filtrate in the ascending limb of the loop of Henle into the surrounding medulla region, raising its osmolarity
- The ascending limb of the loop of Henle is impermeable to water, so water is unable to leave the loop here by osmosis
- The osmolarity of the ascending limb decreases as it rises back into the cortex due to the removal of solutes and retention of water
- The neighbouring descending limb is permeable to water, so water moves out of the descending limb by osmosis due to the high osmolarity of the medulla created by the ascending limb
- The descending limb has few transport proteins in the membranes of its cells, so has low permeability to ions
- The osmolarity of the filtrate increases as the descending limb moves down into the medulla due to the loss of water and retention of ions
- The water and ions that leave the loop of Henle for the medulla make their way into nearby capillaries
- The capillary that flows directly alongside the loop of Henle is known as the vasa recta
- The vasa recta also supplies oxygen to and removes carbon dioxide from the respiring cells of the loop of Henle
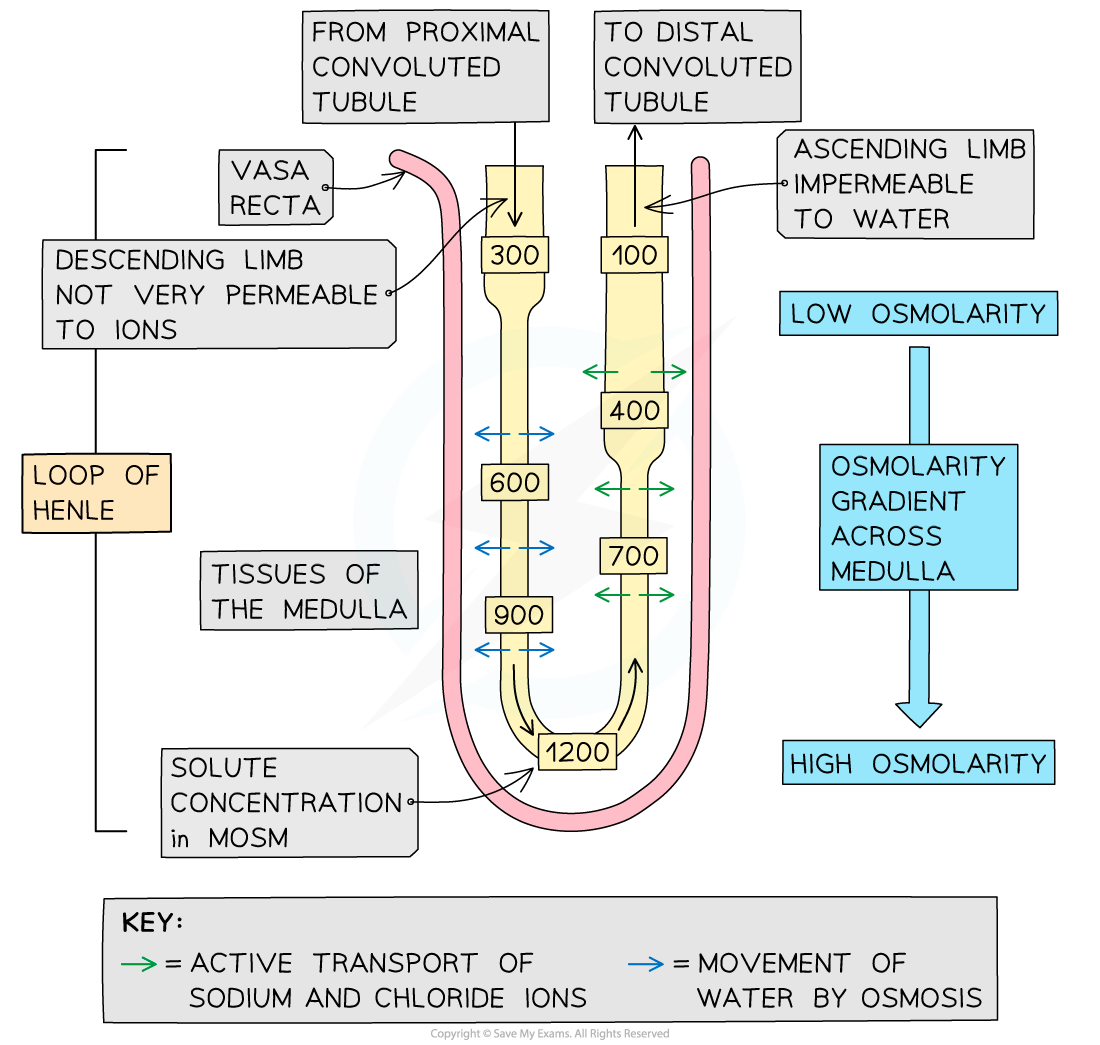
The loop of Henle generates a steep osmolarity gradient across the medulla, maximising the reabsorption of water
