DP Physics Questionbank

C.4 – Medical imaging (HL only)
| Path: |
Description
Nature of science:
Risk analysis: The doctor’s role is to minimize patient risk in medical diagnosis and procedures based on an assessment of the overall benefit to the patient. Arguments involving probability are used in considering the attenuation of radiation transmitted through the body. (4.8)
Understandings:
- Detection and recording of X-ray images in medical contexts
- Generation and detection of ultrasound in medical contexts
- Medical imaging techniques (magnetic resonance imaging) involving nuclear magnetic resonance (NMR)
Applications and skills:
- Explaining features of X-ray imaging, including attenuation coefficient, half-value thickness, linear/mass absorption coefficients and techniques for improvements of sharpness and contrast
- Solving X-ray attenuation problems
- Solving problems involving ultrasound acoustic impedance, speed of ultrasound through tissue and air and relative intensity levels
- Explaining features of medical ultrasound techniques, including choice of frequency, use of gel and the difference between A and B scans
- Explaining the use of gradient fields in NMR
- Explaining the origin of the relaxation of proton spin and consequent emission of signal in NMR
- Discussing the advantages and disadvantages of ultrasound and NMR scanning methods, including a simple assessment of risk in these medical procedures
Guidance:
- Students will be expected to compute final beam intensity after passage through multiple layers of tissue. Only parallel plane interfaces will be treated.
Data booklet reference:
International-mindedness:
- There is constant dialogue between research clinicians in different countries to communicate new methods and treatments for the good of patients everywhere
- Organizations such as Médecins Sans Frontières provide valuable medical skills in parts of the world where medical help is required
Theory of knowledge:
- “It’s not what you look at that matters, it’s what you see.” – Henry David Thoreau. To what extent do you agree with this comment on the impact of factors such as expectation on perception?
Utilization:
- Scanning the human brain (see Biology sub-topic A.4)
Aims:
- Aim 4: there are many opportunities for students to analyse and evaluate scientific information
- Aim 8: the social impact of these scientific techniques for the benefit of humankind cannot be over-emphasized
- Aim 10: medicine and physics meet in the hi-tech world of scanning and treatment. Modern doctors rely on technology that arises from developments in the physical sciences.
Directly related questions
-
16N.3.HL.TZ0.20a:
State the property of protons used in nuclear magnetic resonance (NMR) imaging.
-
16N.3.HL.TZ0.19a:
Show that the attenuation coefficient for bone of density 1800 kg m–3, for X-rays of 20 keV, is about 7 cm–1.
- 16N.3.HL.TZ0.19c: Suggest why more energetic beams of about 150 keV would be unsuitable for imaging a bone–muscle...
-
16N.3.HL.TZ0.19b:
The density of muscle is 1200 kg m–3. Calculate the ratio of intensities to compare, for a beam of 20 keV, the attenuation produced by 1 cm of bone and 1 cm of muscle.
- 16N.3.HL.TZ0.20b: Explain how a gradient field and resonance are produced in NMR to allow for the formation of...
-
17M.3.HL.TZ2.15b:
Describe how an ultrasound transducer produces ultrasound.
-
17M.3.HL.TZ2.15c.i:
Calculate the acoustic impedance Z of muscle.
-
17M.3.HL.TZ1.13c.ii:
the radio-frequency signal emitted towards the patient.
-
17M.3.HL.TZ1.13a:
Outline why the fracture in a broken bone can be seen in a medical X-ray image.
-
17M.3.HL.TZ1.13c.iii:
the non-uniform magnetic field applied to the patient.
-
17M.3.HL.TZ1.13c.i:
the large uniform magnetic field applied to the patient.
-
17M.3.HL.TZ2.15c.ii:
Ultrasound of intensity 0.012 Wcm–2 is incident on a water–muscle boundary. The acoustic impedance of water is 1.50 x 106 kgm–2s–1.
The fraction of the incident intensity that is reflected is given by
where Z1 and Z2 are the acoustic impedances of medium 1 and medium 2.
Calculate the intensity of the reflected signal.
-
17M.3.HL.TZ2.16:
In nuclear magnetic resonance (NMR) imaging radio frequency electromagnetic radiation is detected by the imaging sensors. Discuss the origin of this radiation.
-
17M.3.HL.TZ1.13b:
The diagram shows X-rays incident on tissue and bone.
The thicknesses of bone and tissue are both 0.054 m.
The intensity of X-rays transmitted through bone is Ib and the intensity transmitted through tissue is It.
The following data are available.
Mass absorption coefficient for bone = mass absorption
coefficient for tissue = 1.2 × 10–2m2kg–1
Density of bone = 1.9 × 103 kgm–3
Density of tissue = 1.1 × 103 kgm–3Calculate the ratio .
-
17M.3.HL.TZ2.15a:
State a typical frequency used in medical ultrasound imaging.
- 20N.3.HL.TZ0.18c: Identify one advantage of NMR over ultrasound in medical situations.
- 20N.3.HL.TZ0.17a: Explain how attenuation causes the contrast between soft tissue and bone in the image.
-
20N.3.HL.TZ0.18a:
Explain the cause of the radio-frequency emissions from a patient’s body during nuclear magnetic resonance (NMR) imaging.
- 20N.3.HL.TZ0.17b: X-ray images of other parts of the body require the contrast to be enhanced. State one technique...
-
20N.3.HL.TZ0.18b:
Outline how a gradient field allows NMR to be used in medical resonance imaging.
- 17N.3.HL.TZ0.16a: Show that the attenuation coefficient of lead is 60 cm–1.
-
17N.3.HL.TZ0.16b:
A technician operates an X-ray machine that takes 100 images each day. Estimate the width of the lead screen that is required so that the total exposure of the technician in 250 working days is equal to the exposure that the technician would receive from one X-ray exposure without the lead screen.
-
18M.3.HL.TZ1.14d.ii:
Explain, with appropriate calculations, why a gel is used between the transducer and the skin.
-
18M.3.HL.TZ1.14a:
Outline how ultrasound is generated for medical imaging.
-
18M.3.HL.TZ1.14b:
Describe one advantage and one disadvantage of using high frequencies ultrasound over low frequencies ultra sound for medical imaging.
-
18M.3.HL.TZ1.14d.i:
Calculate the density of skin.
-
18M.3.HL.TZ1.14c:
Suggest one reason why doctors use ultrasound rather than X-rays to monitor the development of a fetus.
-
18M.3.HL.TZ2.15a:
Outline the formation of a B scan in medical ultrasound imaging.
-
18M.3.HL.TZ2.15b.i:
State what is meant by half-value thickness in X-ray imaging.
-
18M.3.HL.TZ2.15b.ii:
A monochromatic X-ray beam of energy 20 keV and intensity I0 penetrates 5.00 cm of fat and then 4.00 cm of muscle.
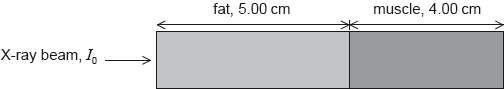
Calculate, in terms of I0, the final beam intensity that emerges from the muscle.
-
18M.3.HL.TZ2.15b.iii:
Compare the use of high and low energy X-rays for medical imaging.
- 18N.3.HL.TZ0.15b: Outline the measurement that needs to be made after the RF signal is turned off.
-
18N.3.HL.TZ0.15c:
Describe how the measurement in (b) provides diagnostic information for the doctor.
-
18N.3.HL.TZ0.16b:
Determine, in terms of I0, the intensity of ultrasound that is reflected at the muscle–bone boundary.
- 18N.3.HL.TZ0.15a: Describe the effect of the RF signal on the protons in the body.
- 18N.3.HL.TZ0.16a: Determine, in terms of I0, the intensity of ultrasound that is incident on the muscle–bone boundary.
- 18N.3.HL.TZ0.16c: Determine, in terms of I0, the intensity of ultrasound that returns to the muscle–gel boundary.
-
19M.3.HL.TZ2.17aiii:
Ultrasound of intensity 50 mW m-2 is incident on a muscle. The reflected intensity is 10 mW m-2. Calculate the relative intensity level between the reflected and transmitted signals.
- 19M.3.HL.TZ2.17aii: Suggest why ultrasound gel is necessary during an ultrasound examination.
-
19M.3.HL.TZ2.17biii:
In the ultrasound scan the frequency is chosen so that the distance between the transducer and the organ is at least 200 ultrasound wavelengths. Estimate, based on your response to (b)(ii), the minimum ultrasound frequency that is used.
- 19M.3.HL.TZ2.17ai: State one advantage and one disadvantage of using ultrasound imaging in medicine compared to...
- 19M.3.HL.TZ2.17bii: Estimate, using data from the graph, the depth of the organ represented by the dashed line.
-
19M.3.HL.TZ2.17bi:
The acoustic impedance of soft tissue is 1.65 × 106 kg m-2 s-1. Show that the speed of sound in the soft tissue is approximately 1500 m s–1.
-
19M.3.HL.TZ2.17biv:
A physician has a range of frequencies available for ultrasound. Comment on the use of higher frequency sound waves in an ultrasound imaging study.
- 19M.3.HL.TZ1.15a: Outline how ultrasound, in a medical context, is produced.
-
19M.3.HL.TZ1.15b:
Suggest the advantage in medical diagnosis of using ultrasound of frequency 1 MHz rather than 0.1 MHz.
-
19M.3.HL.TZ1.16b:
The fluid in the bowel has a similar linear attenuation coefficient as the bowel surface. Gases have much lower linear attenuation coefficients than fluids. Explain why doctors will fill the bowel with air before taking an X-ray image.
-
19M.3.HL.TZ1.16a:
A parallel beam of X-rays travels through 7.8 cm of tissue to reach the bowel surface. Calculate the fraction of the original intensity of the X-rays that reach the bowel surface. The linear attenuation coefficient for tissue is 0.24 cm–1.
- 19M.3.HL.TZ1.15c: Ultrasound can be used to measure the dimensions of a blood vessel. Suggest why a B scan is...
-
19N.3.HL.TZ0.14b:
In nuclear magnetic resonance (NMR) protons inside a patient are made to emit a radio frequency electromagnetic radiation. Outline the mechanism by which this radiation is emitted by the protons.
-
19N.3.HL.TZ0.14a(ii):
State and explain, with reference to you answer in (a)(i), what needs to be done to produce a clear image of the leg artery using X-rays.
-
19N.3.HL.TZ0.14a(i):
Show that the ratio is close to 1.